Biller Experience
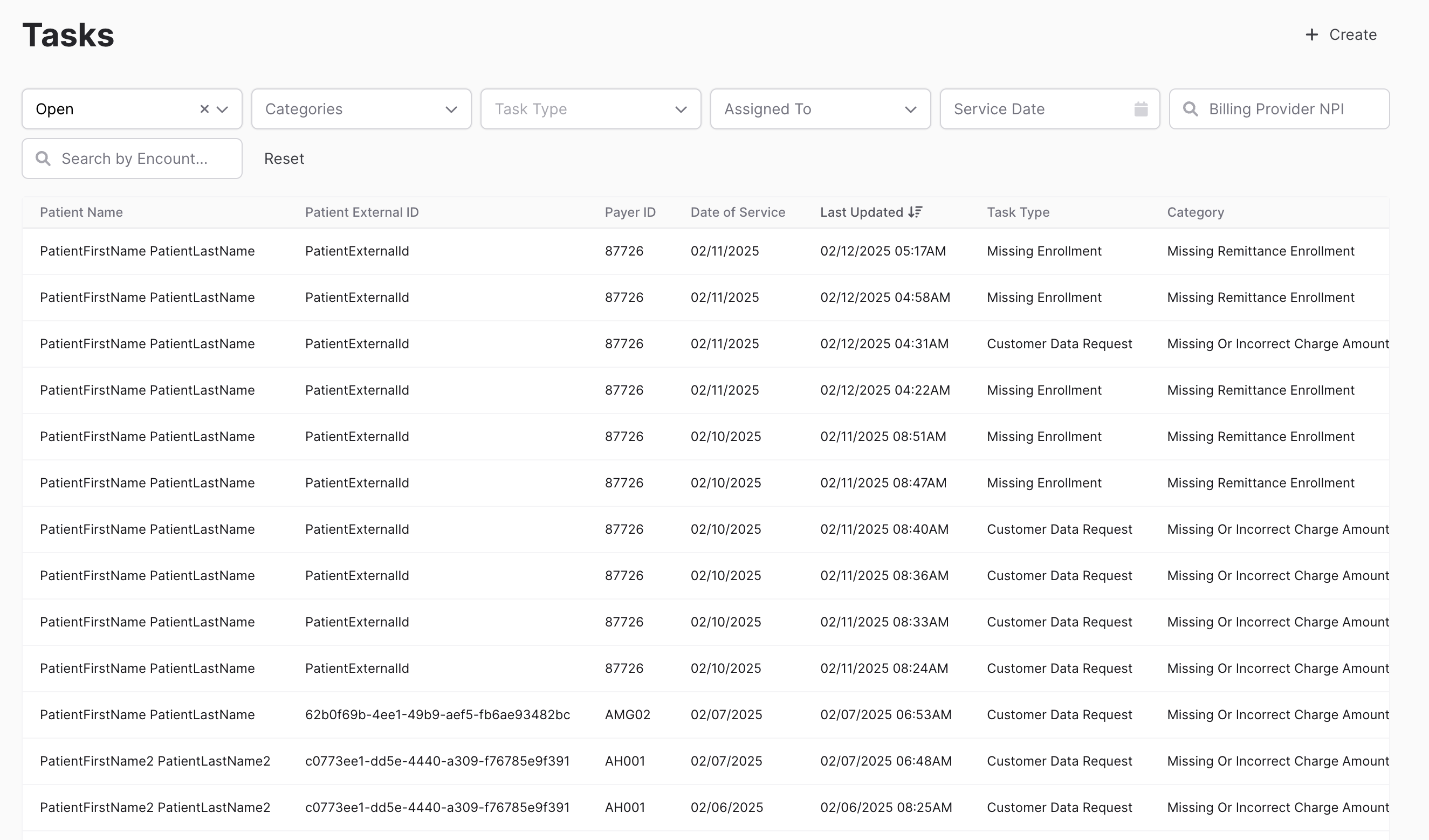
The biller experience encompasses the overall revenue cycle management (RCM) process across the Ottehr EHR. Patients, providers, and billers all play a role in getting insurance claims created and paid. The biller's experience is primarily powered by our partners, Candid (opens in a new tab), for working and submitting insurance claims, and Stripe (opens in a new tab), for payment processing and invoicing.
Let's take a look at how each type of user interacts with the RCM process:
- Patient — During patient registration, patients enter their insurance information and eligibility is checked in real-time so the patient knows what to expect.
- Provider — After the patient visit when the provider reviews and signs the encounter, the claim is automatically created and submitted to Candid.
- Biller — The biller's journey begins when the claim is submitted to Candid. The biller will work on the claim until it is finalized and paid.
Patient Registration
Eligibility Check
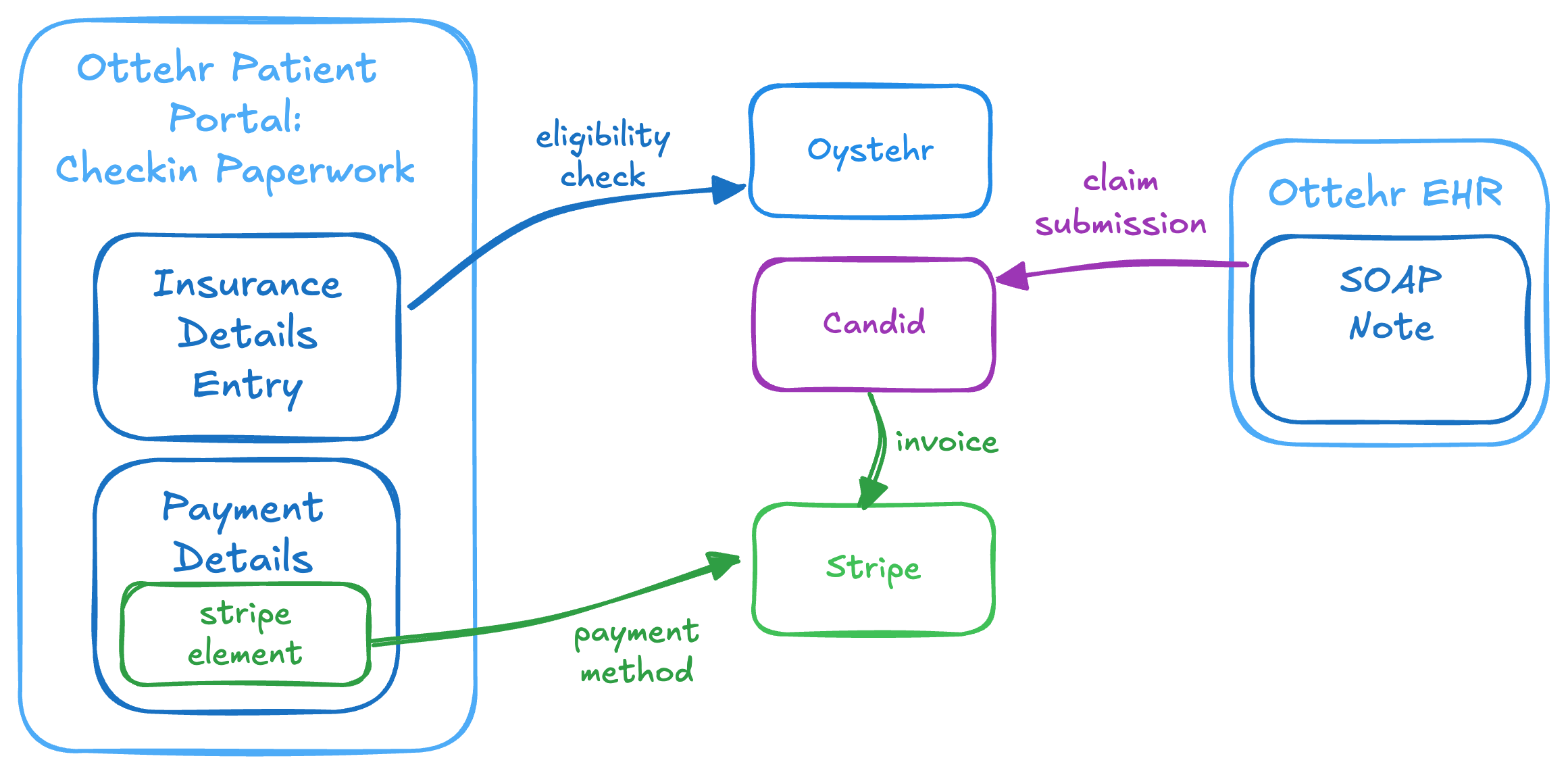
During patient registration, patients enter their insurance information and eligibility is checked in real-time so the patient knows what to expect.
Image: Patient registration insurance information collection and eligibility check
If the patient's insurance passes the eligibility check they continue on to the next step of the registration paperwork. If the patient's insurance does not pass the eligibility check, the patient can navigate back to select the self-pay option.
The eligibility check uses the Oystehr RCM Service Eligibility Check endpoint.
Credit Card Entry
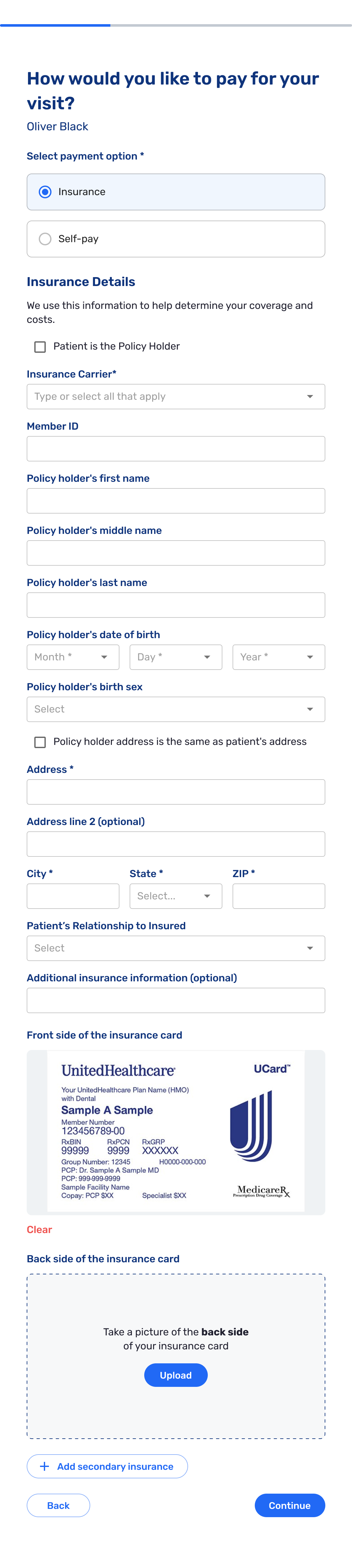
During patient registration, patients are required to enter a credit card.
Image: Patient registration credit card entry
The card is stored securely with Stripe and is used for any patient responsibility payments.
Provider Signs the Chart
When the provider reviews & signs the chart for a visit, Ottehr automatically packages the related details, and creates a Claim in Candid. This is where the EHR leaves off, and the process of working claims picks up with the biller role in Candid.
Biller Works Claims in Candid
The billing team works on the claims in Candid until they are finalized and paid.
The next sections include links to the Candid support portal documentation. If you need access to the Candid support portal, please reach out to us either by email or in Slack (opens in a new tab) and we'll get you set up.
Candid provides excellent "getting started" documentation on how billers work claims pre-submission (opens in a new tab) and post-submission (opens in a new tab).
Claims List
The Claims screen provides a good overview of claims traveling through the revenue cycle:
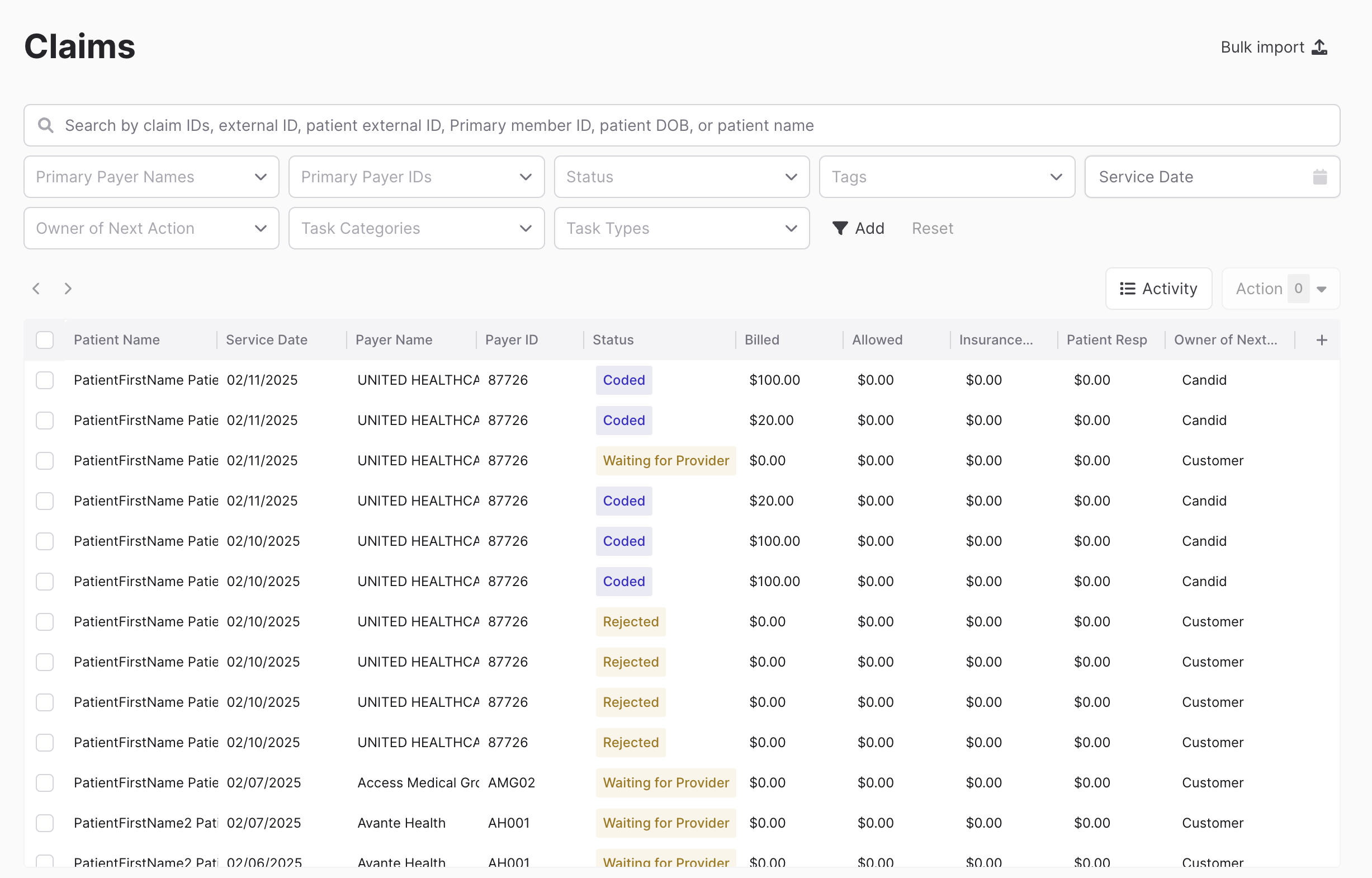
It is important to make a note of the "Owner of Next Action". Finalized claims are labeled as "None" in the owner column and are complete. If the owner of next action is either Candid or Payer, it is being processed and no action is needed from our teams. Claims that are designated for Customer or Coder generally mean that there are inconsistencies or missing data and should be fixed by the biller in Candid.
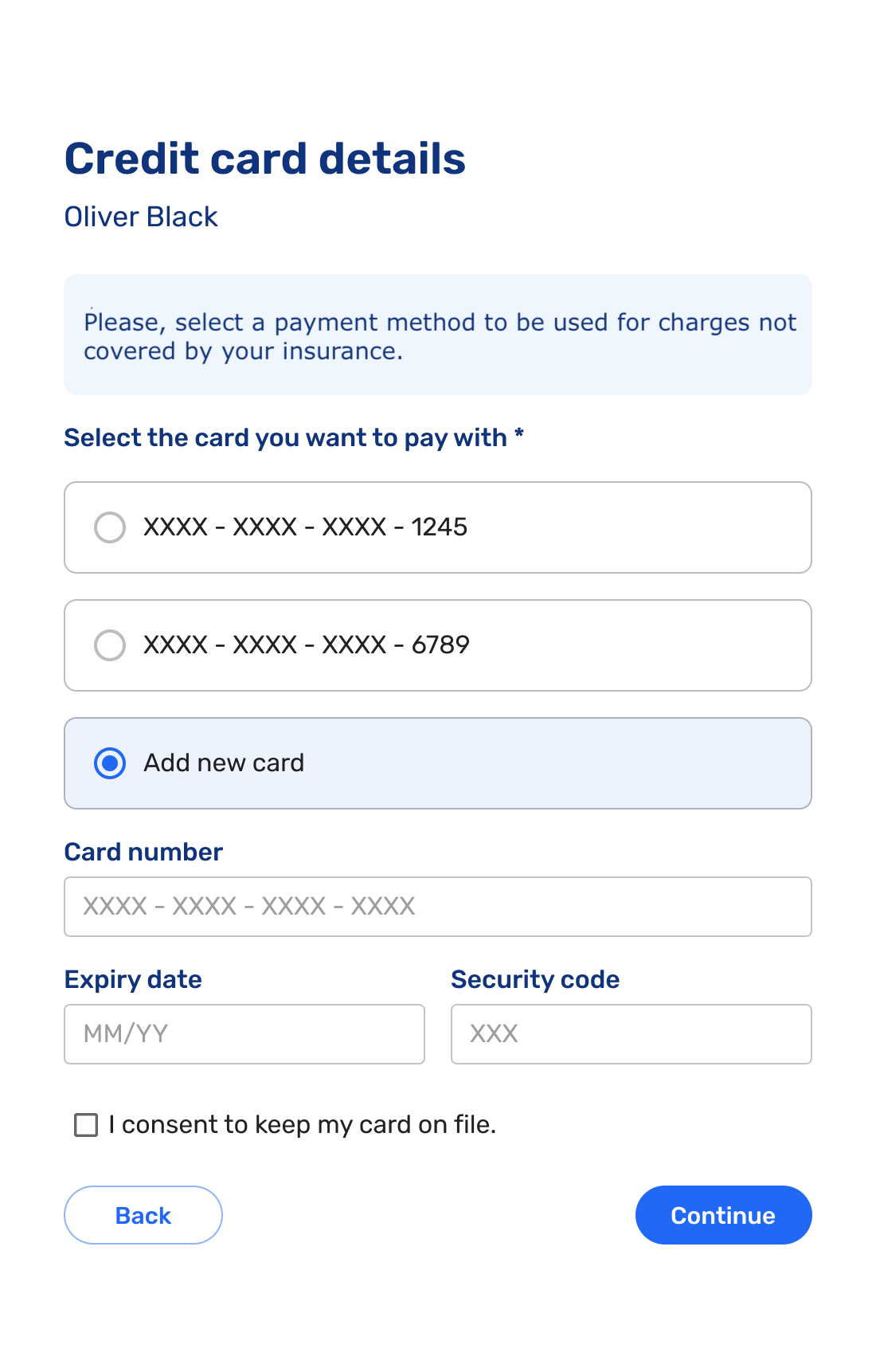
Task List
As claims are submitted to Candid, any errors, including missing or incomplete details, are highlighted, and a task is automatically created by Candid to be resolved by the Biller, by the Oystehr Team, or by Candid itself. The Candid Rules Engine (opens in a new tab) drives creation of tasks, including when tasks will be created and to whom they are assigned. It comes with sensible defaults but can be customized by the billing team to fit their workflow.
The biller can track the tasks in the Candid tasks list.